Free Nursing Notes Templates: With Real Examples
A structured, editable nursing notes template based on the SOAP format. Document patient care clearly with guided sections for subjective, objective, assessment, and plan notes.
Similar Templates
Clear and accurate nursing documentation is essential for patient safety, care continuity, and interdisciplinary communication. The SOAP format is widely adopted in healthcare because it enforces a structured clinical reasoning process—moving from patient-reported symptoms to objective findings, clinical assessment, and actionable care plans.
This nursing notes template is built specifically around that workflow and translates the SOAP method into a practical, interactive form.
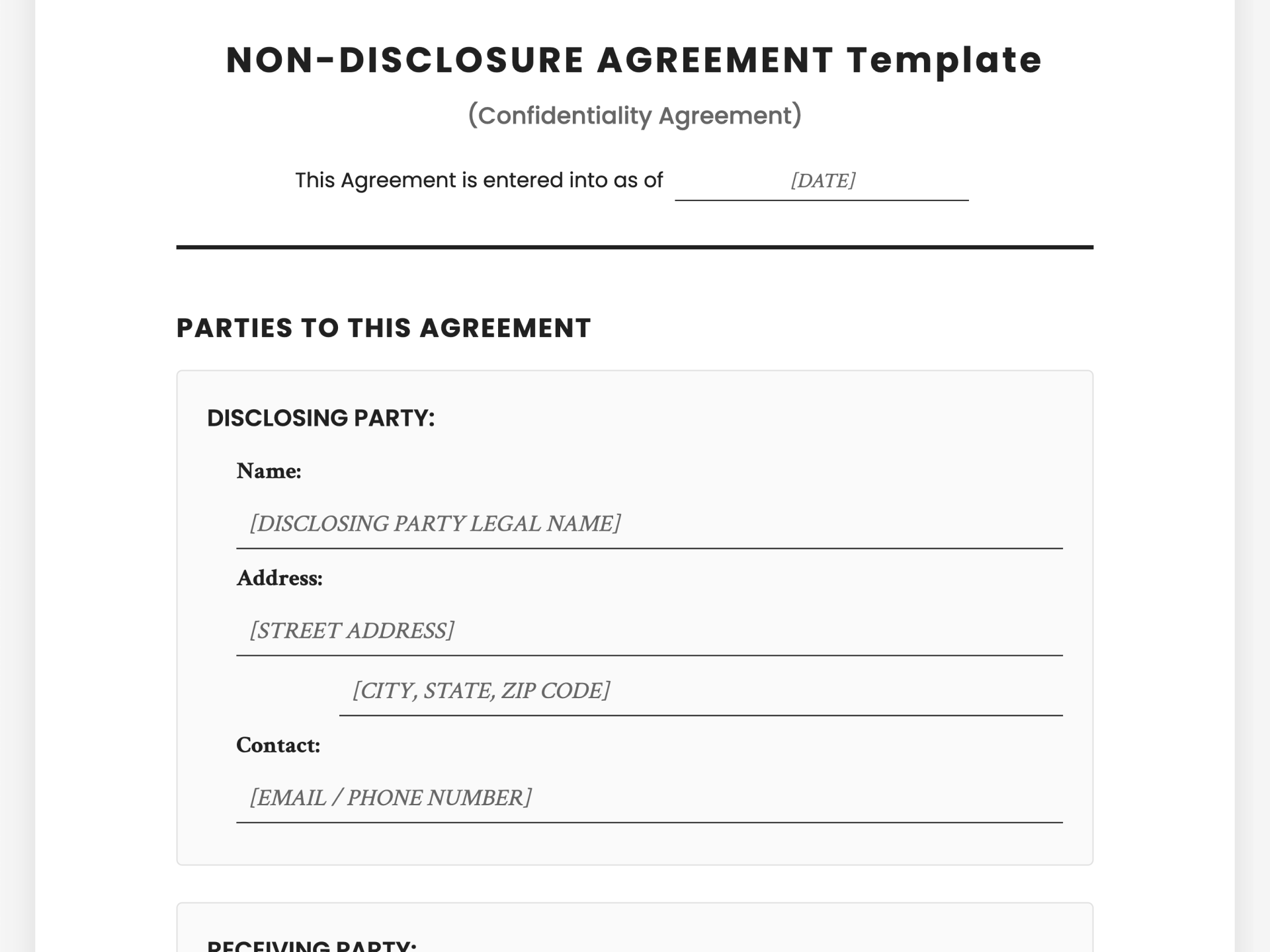
Structured Patient & Encounter Information
At the top of the template, nurses can quickly record essential patient and encounter details, including patient name, medical record number (MRN), date of birth, date, time, and nurse credentials. These fields are clearly separated and formatted to reduce ambiguity and ensure completeness before documentation begins.
This front-loaded structure helps prevent missing identifiers—an issue that often occurs when notes are written under time pressure.
.png)
S — Subjective
The Subjective section focuses on the patient’s own perspective. Instead of an open blank box, the template provides contextual guidance to help nurses document symptoms, concerns, and patient-reported experiences clearly and professionally.
Nurses can record chief complaints, symptom duration, pain descriptions, and the patient’s perception of their condition, all in one dedicated space that aligns with SOAP standards.
O — Objective
The Objective section is designed for measurable, observable clinical data. The template breaks this into structured sub-sections, including vital signs, physical assessment findings, and laboratory or diagnostic results.
By organizing objective data into clearly labeled fields—such as blood pressure, heart rate, temperature, oxygen saturation, and physical exam observations—the template reduces clutter and improves readability for future review by other healthcare professionals.
A — Assessment
In the Assessment section, nurses synthesize subjective and objective findings into clinical judgments. The template encourages clear problem identification, nursing diagnoses, and evaluation of the patient’s response to treatment.
Rather than forcing free-form text, this section is designed to support structured clinical thinking while still allowing flexibility based on patient complexity.
P — Plan
The Plan section focuses on next steps in care. This includes nursing interventions, patient and family education, referrals, follow-up plans, discharge considerations, and expected outcomes.
By keeping all planned actions in one place, the template makes it easier to track care continuity and ensures that nothing critical is overlooked during handoffs or documentation reviews.
Editable, Interactive, and Export-Ready
This nursing notes template is fully editable and interactive. Nurses can type directly into each field, update information as patient conditions change, and reuse the template across different shifts or cases.
Once completed, the notes can be exported as a clean, professional PDF—ideal for documentation submission, training records, or offline reference.
Why Use a SOAP-Based Nursing Notes Template
Using a structured SOAP template helps nurses document more efficiently while improving clarity and clinical accuracy. It reduces the cognitive load of deciding what to write and where, allowing nurses to focus more on patient care and clinical reasoning.
Compared to unstructured notes, SOAP-based documentation improves communication across care teams, supports legal and professional standards, and creates more reliable patient records.
A nursing notes template helps nurses document patient care in a consistent, structured format. It supports clinical communication, legal documentation, and continuity of care across shifts and providers.
SOAP stands for Subjective, Objective, Assessment, and Plan. It is a standardized method used in healthcare to organize clinical documentation logically and clearly.
Yes. The template is well-suited for nursing students, clinical training, and simulation practice because it clearly guides users through each SOAP component with structured sections.
Yes. The template is fully editable and reusable, making it easy to adapt for different patients, departments, or clinical scenarios.
Yes. Once completed, the nursing notes can be exported as a PDF for printing, sharing, or record-keeping.